Investigation of drug-related problems (DRPs) in type 2 diabetes mellitus outpatients at district hospital’s internal clinic at Ho Chi Minh City, Viet Nam
- Cu Chi regional general hospital, Ho Chi Minh City, 700000, Viet Nam
- Faculty of Pharmacy, University of Medicine and Pharmacy at Ho Chi Minh City, 700000, Viet Nam
- Faculty of Pharmacy, Ton Duc Thang University, Ho Chi Minh city, 700000, Viet Nam
- Binh Thanh district hospital, Ho Chi Minh City, 700000, Viet Nam
- District 7 hospital, Ho Chi Minh City, 700000, Viet Nam
Abstract
Introduction: Drug-related problems (DRPs) are prevalent among outpatients and may lead to suboptimal treatment outcomes. Type 2 diabetes mellitus (T2DM) is increasingly common and poses significant challenges to global health and the economy. Patients with T2DM have multiple risk factors for DRPs. This study aimed to determine the types, frequency, and associated factors of DRPs in prescriptions for T2DM outpatients.
Materials and methods: A retrospective study was conducted to collect prescriptions of T2DM outpatients at District hospital’s internal clinic at Ho Chi Minh city, from October 1st to December 31st, 2022. DRPs were determined using the Pharmaceutical Care Network Europe (PCNE) classification, version 9.1. Factors associated with DRPs were analyzed using a multivariate logistic regression model.
Results: A total of 380 prescriptions were included in the analysis. The mean age of the patients was 62.4 years (± 10.4). More than half of the patients were female (59.7%). In total, 636 drug-related problems (DRPs) were identified, with 82.4% of patients experiencing at least one DRP, averaging 1.68 ± 1.38 problems per patient. The most common prevalent DRP was related to dose timing, accounting for 78.9% of the cases. (78.9%). Other types of DRPs were observed at lower frequencies. The drug classes most commonly associated with DRPs were anti-diabetic agents (A10) and cardiac therapy (C01). Polypharmacy, defined as the presence of five or more concurrent medications, was significantly associated with the occurrence of DRPs (p < 0.05).
Conclusion: The proportion of prescriptions with DRP in this study setting was quite notably high. Early identification of the types of DRPs along with related associated factors, is essential. Providing physicians with information about common DRPs may aid in preventing these issues in outpatients with Type 2 diabetes mellitus (T2DM).
Introduction
The term “Drug-related problem” (DRP) was introduced in the early 1990s by Hepler and Strand1. In 2009, Pharmaceutical Care Network Europe (PCNE) defined a DRP as the definition: an event or circumstance involving drug therapy that actually or potentially interferes with desired health outcomes’2. DRPs are prevalent in most healthcare settings and can significantly impact patients, their families, healthcare providers, and the entire health system3. A systematic review reported a median incidence (interquartile range) of DRPs at 70.04 ± 59%, and an average of 3.4 ± 2.8 per patient (interquartile range) in primary healthcare institutions4.
Diabetes is one of the most common non-communicable diseases globally. Diabetic patients face several risk factors that increase their likelihood of experiencing DRPs: advanced age, comorbidities, complications, polypharmacy, etc5. In Vietnam, while the occurrence of DRPs among outpatients has been documented in several recent studies, research specifically focusing on the diabetic population remains limited. This study aims to investigate the categories and proportions of DRPs, as well as the factors associated with DRPs in outpatients with type 2 diabetes mellitus (T2DM) at the Internal Clinic of District Hospital at Ho Chi Minh city.
Materials-Methods
Study population and sampling frame
The study population comprised outpatients with T2DM who were examined at the Internal Clinic of District Hospital at Ho Chi Minh city between October 2022 and December 2022. The sample size was calculated by using Sample Size Calculation for Proportion method is: n = (Z2 x p (1 / p)) / d2 based on the research conducted by of Belayneh et al (2021) 6, with a minimum of 373 patients to give a margin of error = 0.04 (d = 0.04) and a confidence level of 95% (p = 0.05). A minimum sample size of 373 patients was determined to achieve a margin of error of 0.04 (d = 0.04) and a confidence level of 95% (p = 0.05).
Study design and setting
A retrospective study was conducted at the Internal Clinic of District Hospital of Ho Chi Minh city, following approval from by the Hospital Science and Technology Committee (Decision of Science and technology committee at hospital on 29th December 2022). A total of 380 patients who met the inclusion criteria were participated in the study. The primary inclusion criteria for the 380 participants were as follows:
- Aged ≥ 18 years.
- Underwent tests for serum creatinine (SCr), aspartate aminotransferase (AST), and alanine aminotransferase (ALT).
- Prescribed at least one medication for the treatment of T2DM.
Procedure and materials
The method according to the description of Abdulmalik et al (2019) with several modified to suitable in the studies conditions in district hospital. 7 The study was conducted using the Electronic Medical Record System of the hospital. Initially, T2DM outpatients who underwent testing for SCr, AST, and ALT at the Internal Clinic between October 2022 and December 2022 were identified. Prescriptions from these patients who met the inclusion criteria were then collected until a total of 380 prescriptions were reached, employing a convenience sampling method.
Identification of Drug-related problems and risk factors
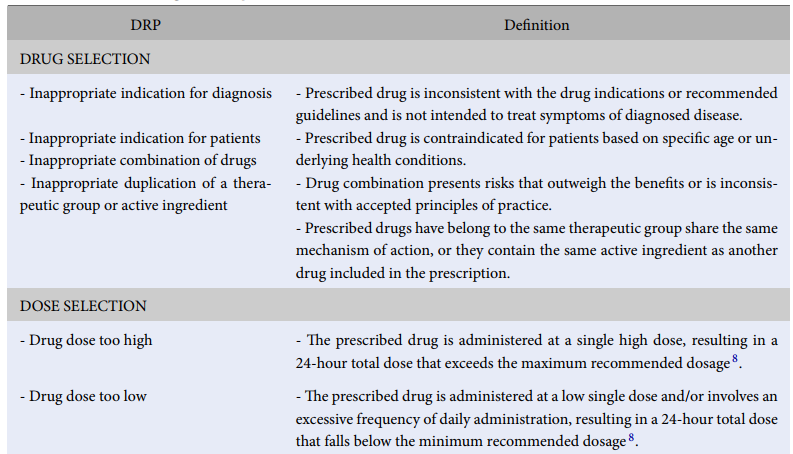
DRPs were identified and categorized using the PCNE classification system, version 9.1. The categories included “drug selection,” “dose selection,” “dosage regimen,” “dose timing,” and “drug usage” (see
Criteria for Drug-related problems identification
|
DRP |
Definition |
|
DRUG SELECTION | |
|
- Inappropriate indication for diagnosis - Inappropriate indication for patients - Inappropriate combination of drugs - Inappropriate duplication of a therapeutic group or active ingredient |
- Prescribed drug is inconsistent with the drug indications or recommended guidelines and is not intended to treat symptoms of diagnosed disease. - Prescribed drug is contraindicated for patients based on specific age or underlying health conditions. - Drug combination presents risks that outweigh the benefits or is inconsistent with accepted principles of practice. - Prescribed drugs have belong to the same therapeutic group share the same mechanism of action, or they contain the same active ingredient as another drug included in the prescription. |
|
DOSE SELECTION | |
|
- Drug dose too high |
- The prescribed drug is administered at a single high dose, resulting in a 24-hour total dose that exceeds the maximum recommended dosage |
|
- Drug dose too low |
- The prescribed drug is administered at a low single dose and/or involves an excessive frequency of daily administration, resulting in a 24-hour total dose that falls below the minimum recommended dosage |
|
DOSAGE REGIMEN | |
|
- Dosage regimen too frequent Dosage regimen not frequent enough |
- The drug is prescribed an excessive frequency of daily administration. - The drug is prescribed an insufficient frequency of daily administration. |
|
DOSE TIMING | |
|
- Dose timing in time of day - Dose timing relative to meals |
- The drug is recommended for administration at specific of the day (morning, noon, afternoon, evening), but the prescription lacks clear instructions or contains incorrect information. - The drug is recommended to be taken before, during, or after meals, but the prescription lacks instructions or contains incorrect or unclear guidance. |
|
DRUG USAGE |
Instructions for administering drugs are missing from the prescription or differ from established recommendations. |
Factors associated with DRPs were identified using multivariable logistic regression models employing the Backward-Forward method:
Dependent variable: Drug-related problem (yes/no)
Independent variables:
1. Age group
2. Patient gender
3. Comorbidity (yes/no)
4. Comorbidity category
5. Renal impairment
6. Polypharmacy
Data analysis
All extracted data were analyzed IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, N.Y., USA). Continuous data that followed normal distribution and exhibited homogeneity of variances were presented as mean ± standard deviation. In contrast, non-symmetrically distributed data or demonstrating heteroscedasticity reported as median values along with minimum and maximum ranges.
Logistic regression analysis was employed to identify factors associated with DRPs using the specified dependent and independent variables. The results were expressed as odds ratios (OR) with a 95% confidence interval and corresponding p-value. Statistical significance was defined at a p-value < 0.05 for this study.
Results
Patient characteristics
The mean age of patients was 62.4 ± 10.4 years, with a higher proportion of non-elderly patients compared to elderly patients. Female patients comprised over 50% of the study population. The majority of patients had an HbA1c ≥ 7.0%, with an average of 7.7 ± 1.7%. Most patients had comorbidities in addition to diabetes, with circulatory system diseases being the most prevalent (91.3%). Twelve patients were diagnosed with chronic renal disease while no patient was diagnosed with liver disease (see
Characteristic population
|
Characteristic |
Number of patients (N =380) |
Percentage |
|
Mean age |
62.4 ± 10.4 | |
|
Age group | ||
|
Non–elderly (< 60 years old) Elderly (≥ 60 years old) |
219 161 |
57.6 42.4 |
|
Gender | ||
|
Male Female |
153 227 |
40.3 59.7 |
|
Drug allergy | ||
|
Yes No |
26 354 |
6.8 93.2 |
|
Comorbidity | ||
|
Yes |
377 |
99.2 |
|
No |
3 |
0.8 |
|
Comorbidity category (according to ICD-10) | ||
|
E (Endocrine, nutritional, and metabolic diseases) I (Diseases of the circulatory system) E (Endocrine, nutritional, and metabolic diseases) I (Diseases of the circulatory system) |
292 356 52 39 115 |
74.9 91.3 13.7 10.3 30.3 |
|
HbA1c | ||
|
Mean < 7.0% ≥ 7.0% |
7.7 ± 1.7 154 226 |
40.5 59.5 |
|
Chronic renal disease | ||
|
Yes No |
12 368 |
3.2 96,8 |
|
Liver disease | ||
|
Yes No |
0 100 |
0.0 100.0 |
Prescription characteristics
The majority of patients exhibited polypharmacy, with an average of 5.2 ± 1.7 medications per patient. Approximately 77.1% of patients were prescribed combination therapies for the treatment of type 2 diabetes mellitus (T2DM), with the combination of metformin and sulfonylureas representing the highest proportion. Among those receiving monotherapy for T2DM, metformin was the first choice (11.6%), followed by sulfonylureas (8.4%). In addition to diabetes medications (A10), agents acting on the renin–angiotensin system (C09), lipid modifying agents (C10), and beta-blocking agents (C07) were also frequently prescribed (see
Prescription characteristic
|
Prescription characteristic |
Number of prescriptions (N = 380) |
Percentage |
|
The mean number of drugs |
5.2 ± 1.7 | |
|
Polypharmacy (≥ 5 medications) Yes No |
238 142 |
62.6 37.4 |
|
Drug group (according to ATC level 2) A10 (Drug used in diabetes) B01 (Antithrombotic agents) C01 (Cardiac therapy) C03 (Diuretics) C07 (Beta blocking agents) C08 (Calcium channel blockers) C09 (Agents acting on the renin-angiotensin system) C10 (Lipid modifying agents) Others |
380 86 69 7 190 104 295 278 144 |
100.0 22.6 18.2 1.8 50.0 27.4 77.6 73.2 37.9 |
|
Monotherapy for diabetes Metformin Sulfonylureas Insulin |
87 44 32 8 |
22.9 11.6 8.4 2.1 |
|
Other |
3 |
0.8 |
|
Combination treatment for diabetes Insulin + oral antihyperglycemic Metformin + sulfonylureas Other |
293 45 234 14 |
77.1 11.8 61.6 3.7 |
Drug-related problems
Category of Drug-related problems
|
Category |
Number of DRP (N = 636) |
Percentage |
|
Drug selection - Inappropriate indication for diagnosis - Inappropriate indication for patients - Inappropriate combination of drugs -Inappropriate duplication of the therapeutic group or active ingredient |
29 6 6 1 16 |
4.5 0.9 0.9 0.2 2.5 |
|
Dose selection - Drug dose too high - Drug dose too low |
40 4 36 |
6.3 0.6 5.7 |
|
Dosage regimen - Dosage regimen too frequent - Dosage regimen does not frequent enough |
51 41 10 |
8.0 6.4 1.6 |
|
Dose timing - Dose timing in time of day - Dose timing relative to meals |
502 21 481 |
78.9 3.3 75.6 |
|
Drug usage |
14 |
2.2 |
A total of 82.4% of patients (n = 380) had at least one DRP. In total, 636 DRPs were identified, yielding a mean of 1.68 ± 1.38 DRPs per patient. Among the determined DRPs, dose timing accounted for the highest proportion at 78.9%, while the remaining DRPs represented insignificant proportions. A detailed classification of the identified DRPs among the 380 subjects is presented in
The drug classes most likely to contribute to DRPs including medications used in diabetes (A10) which accounted for 72.6%, followed by cardiac therapy (C01) at 10.2%. A list of specific medications associated with DRPs is also provided in
Medication categories involving drug-related problems
|
Number |
Drug group |
Number of DRP (N = 636) |
Percentage |
|
1 |
A10 (Drug used in diabetes) |
462 |
72.6 |
|
2 |
B01 (Antithrombotic agents) |
44 |
6.9 |
|
3 |
C01 (Cardiac therapy) |
65 |
10.2 |
|
4 |
C03 (Diuretics) |
4 |
0.6 |
|
5 |
C07 (Beta blocking agents) |
2 |
0.3 |
|
6 |
C08 (Calcium channel blockers) |
1 |
0.2 |
|
7 |
C09 (Agents acting on the renin-angiotensin system) |
4 |
0.6 |
|
8 |
C10 (Lipid modifying agents) |
2 |
0.3 |
|
9 |
Others |
52 |
8.3 |
Factors associated with Drug-related problems in type 2 diabetes mellitus patients
Factors associated with drug-related problems
|
Factor |
OR |
95% CI (OR) |
p |
|
Age group | |||
|
< 60 years old ≥ 60 years old |
1 1.33 |
0.74 – 2.40 |
0.347 |
|
Gender | |||
|
Male Female |
1 0.83 |
0.47 – 1.47 |
0.52 |
|
Comorbidity | |||
|
No Yes |
1 3.16 |
0.23 – 42.7 |
0.387 |
|
E (Endocrine, nutritional, and metabolic diseases) | |||
|
No Yes |
1 0.60 |
0.30 – 1.22 |
0.16 |
|
I (Diseases of the circulatory system) | |||
|
No Yes |
1 0.83 |
0.28 – 2.45 |
0.73 |
|
K (Diseases of the digestive system) | |||
|
No Yes |
1 0.79 |
0.36 – 1.71 |
0.55 |
|
M (Diseases of the musculoskeletal system and connective tissue) | |||
|
No Yes |
1 1.10 |
0.38 – 3.11 |
0.87 |
|
Renal impairment | |||
|
No Yes |
1 1.72 |
0.18 – 15.83 |
0.63 |
|
Other disease | |||
|
No Yes |
1 0.94 |
0.46 – 1.91 |
0.86 |
|
HbA1c | |||
|
< 7.0% ≥ 7.0% |
1 1.37 |
0.78 – 2.40 |
0.27 |
|
Polypharmacy | |||
|
No Yes |
1 3.09 |
1.53 – 6.23 |
0.002 |
Factors associated with DRPs were identified using multivariable logistic regression models employing the Backward-Forward method. The independent variables included:
1. Age group
2. Patient gender
3. Comorbidity (yes/no)
4. Comorbidity category
5. Renal impairment
6. Polypharmacy
After assessing for multicollinearity, the variance inflation factor (VIF) values for all independent variables were found to be less than 2 and allowing for the inclusion of all variables in the regression model.
The results of the logistic regression analysis, as shown in
Discussion
Patient characteristics
The mean age of the population was 62.4 ± 10.4 years, with the youngest participant aged 27 years and the oldest 99 years. The proportion of elderly patients was higher than that of non-elderly patients. This finding is comparable to a study by Truong Tran Anh Thu (2019), which reported a mean age of patients was 63.4 ± 11.3 years, with elderly individuals comprising 54.0%9of the sample. The geriatric population is at high risk for DRPs due to multi-morbidities, polypharmacy, and pharmacokinetic, and pharmacodynamic changes associated with aging10. In this study, 99.2% of T2DM patients had at least one comorbidity.
Regarding comorbidities, most patients had additional diagnosis aside from T2DM. Among those comorbidities, group I and E (according to ICD-10) represented the highest proportion. This aligns with Vietnam’s disease profile, where non-communicable diseases account for over 70% of the disease burden, with hypertension and diabetes being leading causes of mortality11. Previous studies by Zaman Huri H. (2013), Sharma A. (2018), and Mechessa D. F. (2020) also showed that common comorbidities in T2DM patients, including hypertension, cardiovascular disease, stroke, dyslipidemia, and renal impairment12, 13, 14. However, in this study, only 3.2% of patients were diagnosed with renal impairment15. A similar study by S. Z. Inamdar (2016) reported that T2DM patients with renal impairment constituted 0.5% of the sample. Differences in race, epidemiology, lifestyle, ability to access treatment, and awareness of illness may contribute to these varying proportions16.
In terms of glycemic control, the majority of participants had an HbA1C ≥ 7.0% (59.5%). This result consistent with findings from by Zaman Huri H. (2013), which indicated that 73.0%13of patients did not achieve target glycemic control. Poor glycemic control has also been identified as a risk factor associated with DRPs in the previous studies14.
Prescription characteristics
A significant 62.6% of participants were identified as experiencing polypharmacy with the mean number of medications amounting to 5.2 ± 1.7. This finding aligns with the observation that most patients had comorbidities, necessitating the use of multiple medications. In contrast, the study conducted by Yihama M. (2018) reported different results, with a mean of 4.08 ± 1.15 medications and only 34% of participants taking more than 5 drugs. This discrepancy may be attributed to the fact that only 23.3% of patients in Yihama's study had at least one comorbidity17.
The combination of metformin and gliclazide was the most prevalent in combination therapy, while metformin itself was the most commonly prescribed medication for monotherapy in the treatment of T2DM.
Insulin was prescribed in both monotherapy and combination therapy, albeit for a smaller proportion of patients. Yihama M. (2018) similarly found that metformin was the most frequently indicated medication for both monotherapy and as part of combination therapy, with metformin-glibenclamide being the most common combination. Additionally, a study by Kefale B. (2013) reported comparable findings, indicating a low prescription rate for insulin and its combinations with oral antihyperglycemic agents.
Differences in medication prescriptions may arise from variations in patient characteristics, as well as factors related to the accessibility and affordability of insulin.
The combination of metformin and gliclazide was the most prevalent in combination therapy, while metformin itself was the most commonly prescribed medication monotherapy in the treatment of T2DM. Insulin was prescribed in both monotherapy and combination therapy, but for a minor proportion of patients. Yihama M. (2018) similarly found that metformin was the most frequently indicated medication for both monotherapy and as part of combination therapy – with metformin-glibenclamide being the most common17. Additionally, a study by Kefale B. (2013) reported comparable findings, indicating a low prescription rate18for insulin and its combinations with oral antihyperglycemic agents. Differences in medication prescriptions may arise from various in patient characteristics, as well as factors related to the accessibility and affordability of insulin19.
Drug-related problems
This study recorded a total of 636 DRPs, with 82.4% of prescriptions associated with at least 1 DRP and the mean number of DRPs per patient was 1.68 ± 1.38. These findings are comparable to those of Duong Thi Ly Huong (2023), who reported a DRP prevalence of 74.3% and a mean of 1.54 ± 1.07 DRPs per patient20. In contrast, the study by Abu R. K. (2018) indicated a significantly higher mean number of DRPs, recorded at 6.3 ± 2.121. All these studies focused on diabetic outpatients. The variance in results can be attributed to several factors, including the disease model of hospitals and population, variations in the classification used in studies (PCNE, Nil, Cipolle, Hepler, and Strand), type and quantity of references, the intervention of clinical pharmacists.
Dose timing was identified as the most prevalent category of DRP in this study, accounting for 78.9%. This finding aligns with research from Le Thanh Tam et al (2022) which reported similar outcome22. Additionally, research by Nguyen Anh Nhut el al (2019) identified inappropriate dosage as the most common DRP, followed by timing of administration23. All these studies focused on outpatients. International studies have also highlighted dosing, drug choice, and adverse reactions as the most common categories for DRP24. Variations in the proportion of DRPs may be attributed to the following factors. First, the version of PCNE classification utilized in this study was 9.1, while Chung A. Y. (2019) employed version 5.01. These differing versions include modifications and updates that may affect the classification outcomes. Second, this study primarily reviewed prescriptions and limited patient tests, whereas previous studies often incorporated health record reviews and patient interviews to assess various aspects, including drug-use processes, treatment effectiveness, and adverse reactions, etc.
Further supporting the findings, a study by Le Tran Thanh Vy et al (2021) also identified dose timing as the most common DRP8. A study by Nguyen Anh Nhut et al (2019) indicated that approximately 50% of prescriptions exhibited DRP related to dose timing in relation to meals23. These results suggest that issues with dose timing are prevalent in prescribing practices in Vietnam. According to Nguyen Anh Nhut et al (2019), physicians often overlook the timing of administration during prescrriptions23. In contrast, Wolf C. et al (2015) noted that dose timing is less likely to result in significant harm to patients25.
Metformin, sulfonylureas, and diuretics can affect the timing of DRP throughout the day Metformin and sulfonylureas manufactured in specific dosage formulations like extended-release (XR) or modified-release (MR) typically need to be taken at a particular time. However, these medications were instructed to be used like regular dosage forms in collected prescriptions. Regarding diuretics, some prescriptions had
indapamide specified to be taken in the evening, while indapamide was recommended to be used in the morning to avoid nocturnal urination affecting patient sleep26. Some studies have shown that diuretics can increase the risk of falls in the elderly. The probability of falls in older adults who used diuretics was 1.185 times higher than in patients who did not take diuretics 27. As the majority of the population in this study were older adults, if diuretics are taken at night, the likelihood of causing falls may become greater due to sleep disturbance.
Dose timing relative to a meal can also affect some aspects of the treatment process. In terms of treatment effectiveness, the time of administration influences the pharmacokinetics and pharmacodynamics of medications. Mixed insulin and gliclazide were recommended to be used before meals to improve postprandial blood glucose levels. Antacids should be taken with or soon after meals, because these medicines are used to prevent heartburn, indigestion, and acid reflux. This is the timepoint when patients are most likely to experience heartburn or indigestion. To reduce undesirable effects, metformin or NSAIDs are suggested to be used after meals. For the examples provided, most of the prescriptions lacked instructions or were not clearly instructed. This can lead to ineffective or unsafe treatment, new health problems, and potentially increased treatment costs28.
Dosage regimen was the second most common DRP, accounting for 17.1% of DRPs. This type of DRP was only found in sulfonylureas. Physicians often prescribed glimepiride or gliclazide modified MR two or three times per day, while recommendations suggest once daily dosing. Similarly, drugs in group cardiac therapy caused DRP dosage regimens to be not frequent enough, such as with ivabradine, nicorandil, or trimetazidine (MR form). Physicians prescribed the MR form of trimetazidine twice a day, when the trimetazidine-coated tablet form is recommended to be taken 3 times daily. These problems may be due to variation in prescribing habits among physicians. Differences in health expenditure and patient outcomes can be linked to this variation in clinical practice. Some factors that could be modified to promote more effective prescribing include knowledge, educational level, experience, the number of practicing professionals, cost sharing, and guidelines29.
Owing to collecting test information, this study recorded six prescriptions with medications that were inappropriate for patients due to contraindications for renal impairment patients (CrCl < 30 ml/min) or whose prescribed dosage was higher than the recommendation for renal impairment. Physicians and clinical pharmacists should exercise greater caution when prescribing for special patient populations to prevent potential adverse drug events from overdosing.
The drug classes most likely associated with DRPs were those used in diabetes and cardiac therapy. A study by Kefale B. et al (2020) also found anti-diabetic medications, statins, and aspirin to be the most frequently involved in drug therapy problems18. These results were plain because these are among the most commonly prescribed drugs for treating diabetes, comorbidities, and complications30, 31. Insulin and oral antihyperglycemic medications have been shown to be important risk factors contributing to DRPs32. Therefore, it is evident that physicians and clinical pharmacists play crucial roles in preventing and minimizing DRPs, particularly at the prescribing and patient education stages.
Factors associated with Drug-related problems
Polypharmacy was a risk factor that contributed to the occurrence of DRP in this study. Different previous studies on T2DM patients have appointed similar results12, 13, 14. Diabetic patients often have comorbidities and complications, leading them to take multiple medications for their treatment. Research has shown that each additional medication can increase the number of DRPs33by 8.6%. T2DM patients tend to receive more drugs than their non-diabetic counterparts, making them more susceptible to drug–drug or food–drug interaction34. DRPs due to polypharmacy can increase treatment costs and hospitalizations35. Therefore, practical strategies are needed in T2DM management to prevent polypharmacy and its associated problems, while still ensuring treatment effectiveness for patients.
Limitations
This study did not assess relevant laboratory tests to comprehensively review drug choice and dosing, as diabetic patients often have comorbidities like dyslipidemia and hypertension.
With retrospective study design, this study did not allow the researchers to directly engage with patients to consider DRPs in the treatment process and effectiveness.
Clinical severity has not been evaluated, limiting the ability to propose appropriate intervention measures.
Conclusions
The study was conducted on 380 T2DM outpatients with the largest percentage of total population over 65 years and identified 636 DRPs with 82.4% of patients experiencing at least one DRP and 1.68 ± 1.38 DRPs per patient. The most frequent category of DRP was time dosing (78.9%). Drugs used in diabetes and cardiac therapy were commonly involved in DRP. Polypharmacy was a significant risk factor associated with DRPs. Physicians and clinical pharmacists play crucial roles in preventing and minimizing DRPs, particularly at the prescribing and patient education stages. Future studies should be expanded to determine various causes of DRPs and address the research limitations. The clinical pharmacy department should provide information about common DRPs and drugs involved to physicians, so clinical pharmacy and doctor can consider these factors carefully when prescribing.
Abbreviations
DRPs: Drug-related problems, T2DM: Type 2 diabetes mellitus, PCNE: Pharmaceutical Care Network Europe, A10: Anti-diabetic agents, C01: Cardiac therapy, SCr: Serum creatinine, AST: Aspartate transaminase, ALT: Alanine transaminase, EMR: Electronic Medical Record, SPSS: Statistical Package for the Social Sciences, OR: Odds Ratio, ATC: Anatomical Therapeutic Chemical Classification System, HbA1c: Glycated hemoglobin, ICD-10: International Classification of Diseases, 10th Revision, VIF: Variance Inflation Factor, XR: Extended-release, MR: Modified-release, NSAIDs: Nonsteroidal anti inflammatory drugs, CrCl: Creatinine clearance.
Acknowledgements
The authors are grateful for the support of the board of directors and staff of District 7 hospital.
Author’s contributions
Conceptualization and investigation: Ngan Ha Le, Ngoc Phuc Nguyen, Minh Thanh Nguyen; Formal analysis: Minh Thanh Nguyen, Ngan Ha Nguyen, Ngoc Phuc Nguyen; Validation and data curation: Duc Toan Pham, Huynh Nhu Mai; Writing-Original draft: Minh Thanh Nguyen, Ngan Ha Le, Thi Yen Vy Nguyen; Writing-review and editing: Huynh Nhu Mai, Minh Tien Nguyen, Thi Anh Thi Nguyen, Ngoc Phuc Nguyen. All authors read and approved the final manuscript.
Funding
None
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
A retrospective study was conducted at the Internal Clinic of District Hospital of Ho Chi Minh city, following approval by the Hospital Science and Technology Committee (Decision of Science and technology committee at hospital on 29December, 2022).
Consent for publication
Written informed consent was obtained from the patient for publication of this article and any accompanying images.
Competing interests
The authors declare that they have no competing interests relevant to the study.

