Associating demographic, clinical, and radiological presentation of HIV patients with TB and other co-infections in KPK, Pakistan
- State Key Laboratory of Virology, College of Life Sciences, Wuhan University, Hubei, China
- Department of Biotechnology, Faculty of Chemical and Life Sciences, Abdul Wali Khan University Mardan (AWKUM), Mardan 23390, Pakistan
- Department of Microbiology, Shaheed Benazir Bhutto Women University, Peshawar, Pakistan
- Department of Nursing, Shifa Tameer-e-Millat University, Islamabad, Pakistan
- Department of Nursing, Nishtar Medical University, Multan, Pakistan
- Department of Nursing, Shalamar Institute of Health Sciences, Lahore, Pakistan
- Department of Nursing, Allama Iqbal Medical College, Lahore, Pakistan
Abstract
Background: The human immunodeficiency virus (HIV) afflicts the immune system by annihilating the white blood cells. The infection of HIV can alter the epidemiology and clinical profile of tuberculosis (TB) in patients suffering from co-infection. The objectives of the current study were to demographically and retrospectively analyze the data of HIV-infected patients admitted to different hospitals at KPK, Pakistan, and elaborate the key radiological and clinical differences in HIV positive patients with various co-infections and their effect on the CD4 level.
Methodology: Initially, 1057 patients with HIV admitted to different hospitals of KPK were assessed for clinical presentation, co-infections, and their correlation with CD4 level. The data of patients, including date of hospital registration, weight, gender, diagnosis, age, and therapy, were obtained using a specifically designed Performa. In addition, sputum test of HIV patients was also conducted for screening of TB.
Results and Conclusion: Our main findings are that HIV makes TB more severe such that CD4 count cell reduces to a level of 82-120 (killer stage). The incidence of HIV is two times greater in the males of the population under study. Young, single, and illiterate males were more affected by HIV and TB due to sexual contact and injecting intravenous drugs by contaminated syringes. Radiography was abnormal and pulmonary TB was common in HIV-positive TB patients. Co-infection of HIV and TB significantly reduced CD4 cells level in patients. The majority of HIV patients were Afghan refugees or those who came to Pakistan for better treatment.
INTRODUCTION
Tuberculosis is a long-term infectious disease caused by the bacteria Mycobacterium tuberculosis bacillus (Koch bacillus), whose major features include a predilection for lung parenchyma and dissemination from person to person through inhalation of a microorganism containing particles 1. Tuberculosis is one of the most common infections associated with HIV infection 2. Other research among HIV-positive TB patients shows that tuberculosis is a frequent opportunistic infection in HIV-positive individuals, with a significant frequency of pulmonary and extrapulmonary tuberculosis, as well as complex clinical presentations3. Clinical symptoms, sputum smear testing for acid-fast bacilli (AFB), tuberculin skin test, and chest radiography are used to diagnose pulmonary TB in most impoverished countries4. AIDS was first recognized in 1981;AIDS had a significant impact on the global TB issue as it changed its epidemiology and made containment more challenging5. In 2019, around 38 million individuals were living with HIV/AIDS worldwide6. There were 36.2 million adults and 1.8 million children (15 years old). Tuberculosis affects over 2 million individuals per year, and management methods are vulnerable to early detection, drug resistance, and the socioeconomic conditions7. Infection with the human immunodeficiency virus (HIV) is a major risk factor for disease progression in those who have already been infected with the bacillus. While the likelihood of an infection developing to TB illness in immune-competent persons is 10% throughout their lifetime, it is likely to be 8 to 10% in HIV-negative infected individuals annually8. Furthermore, it is the earliest and most serious consequence among HIV-positive people, occurring before other public diseases. Clinical and radiographic differences between HIV-positive and HIV-negative individuals with tuberculosis have to be identified in studies. According to the World Health Organization (WHO), 4.4 million persons worldwide have dual infections with tuberculosis and HIV, with almost 80 % of these people living in various areas9, 10. One-third of all HIV/AIDS patients are also infected with . HIV is making the TB epidemic considerately eviler and has been the only significant factor determining the increased number of TB cases. In HIV-positive patients with CD4 counts > 200, radiographic discoveries are seen as infiltration and cavitations in upper lobes similar to tuberculosis in HIV-negative persons12. In HIV-positive patients with CD4 sum < 200 mediastinal adenopathy and pleural effusion are common, which is the same as the condition seen in HIV-negative patients with primary infection 13, 14, 15. With molecular epidemiologic methods, it is proved that the presence of adenopathy does not necessarily represent primary infection, but it might probably be due to immunodeficiency16. About 5% of HIV-positive patients have normal radiography despite positive patients’ sputum culture17.
Severity in HIV lead to interest to study more about HIV and its co-infections, which result to sort out many co-infections caused by HIV accept TB that includes people with HIV are disproportionately impacted by viral hepatitis; about one-third of HIV patients are co-infected by either HBV or HCV, that can result in long-term illness and mortality18. The second most important co-infection is malaria HIV infection had an unpredictably enormous relationship with the effect of malaria in a region of unstable transmission19. Diarrhea is also a general complication of HIV infection;30-90% of patients with AIDS suffer from diarrhea at some point of their illness and detection of etiologic agents 20.
The goal of the current research was to demographically and retrospectively analyze the data of HIV-infected patients admitted to different hospitals at Peshawar and Kohat, KPK, Pakistan. The key radiological and clinical differences in HIV-positive patients with various co-infections and their effect on CD4 levels were also elaborated.
MATERIAL AND METHODS
Ethical Approval of the study
The Department of Zoology at Kohat University of Science and Technology in Pakistan, the Department of Microbiology at Khyber Medical University in Peshawar, Pakistan, the Department of Microbiology at Shaheed Benazir Bhutto Women University in Peshawar, Pakistan, and the AIDS control program in KPK gave approval for the study.
Study zone and sample collection
The study was conceded out of different hospitals in Khyber Pakhtunkhwa, Pakistan, including Khyber Teaching Hospital, Hayatabad Medical Complex, Kohat Medical College, and Lady Reading Hospital Peshawar. Initially, a retrospective study was conducted on HIV patients admitted to these hospitals for 8 years (January 2012 – December 2019). The medical and microbiological records were analyzed. The data of patients, including date of hospital registration, weight, gender, diagnosis, age, and therapy, were obtained using a specifically designed Performa. Sputum test of HIV patients was also conducted for screening of TB.
The sample was collected from KPK hospitals according to 5 different categories.
-
Gender: About 1057 patient samples were taken according gender-wise and divided into 4 categories i.e.,male, female, children, and infants
-
Age: Out of 1057, samples were taken out according to age gap that includes: 10-20, 21-30, 31- 40, and > 40 and were studied
-
Area: According toarea-wise distribution, patients were divided into the following groups: KPK, Fata, Attock, Afghani, and Prisoners
-
Demographic: The demographic and clinical variables were set, which were common in KPK that include mainly fever, weight loss, cachexia, diaphoresis, and diabetes in 1057 patients.
-
CD4 Level: The level of CD4 cells in HIV patients concerning co-infection was also determined.
The BD FACS System was used to acquire absolute CD4+ levels in the sample 21.
Sputum
It includes a sputum test on which microscopy, Zhel-nelson staining, and Elisa was performed. Out of 1057 sputum models, 153 were obtained directly from the patients in a clean and sanitized sputum vessel and correctly labeled. Then, all of the samples were taken to the Molecular Parasitology and Virology Lab, Department of Zoology, Kohat University of Science and Technology's AIDS Control Program in KPK, Kohat, for TB diagnosis.
The yellowish part was trawled out from the sputum flask and placed on a slide with an uneven stick. The material was uniformly spread on a slide in an approximate area of 2cm-1cm for comprehensibly drying. The smear was then completely dried and heat fixated.

Number of patients suffering from various types of HIV co-infections (* = HIV co-infection with significant number of patients)

Comperative analysis of average level of CD4 cells (cells/mm3) in HIV positive patients with different co-infections
Radiological and sputum test results representing involment of different sites of TB among HIV positive TB patients

Regional and populational representation of HIV infected patients
Ziehl-Neelsen staining
The prepared slides were then placed on the staining chamber, which contained Carbol Fuchsin, and left for about 5-10 minutes. For fixing, the heat was provided through a spirit lamp. After cooling of slides, a little amount of decolorizing agent was added. It was followed by washing with usual tape water. The slide was once again dipped in the second box, which contained methylene blue for 5-10 minutes. The prepared smear was observed under the oil immersion microscope at 10xs, 40xs, and 100xs and acknowledged with the regular images. Slides with red rods against the blue background show the existence of (TB).
Statistical Analysis
Constant data was characterized by the mean (SD), while the frequency and percentages represented categorical data. The mean of continuous variables in three classes is compared using a one-way ANOVA. In categorical factors, the chi-square was used to determine the mean. Significant was described as a P value of 0.05 or less. Microsoft Excel 2016 and the SPSS statistical program version 15 were utilized to analyze the data.
1. RESULTS
Retrospective, Demographics and Clinical analysis
The retrospective analysis revealed that a total of 1291 HIV patients were admitted to hospitals of KPK from January 2012 – December 2019, out of which 234 were eliminated due to lack of data, who were not willing to participate, or patients with age less than 15. Of 1057 HIV patients, 74.14% were males with ages ranging between 21- 30 (77.95%). The majority of the infected patients were single and illiterate (79.71% and 78.33%, respectively). In the current study, injecting drugs by utilizing contaminated syringes and sexual relationships with the infected person were the significant viral transmission route in patients (
Demographic and retrospective analysis of HIV patients admitted tovarious hospitals of Peshawar and KPK
|
Total |
Samples |
Male |
Female |
Male % |
Female % |
|
1057 |
784 |
273 |
74.17% |
25.83% | |
|
Age | |||||
|
15-20 |
110 |
71 |
39 |
64.55% |
35.45% |
|
21-30 |
458 |
357 |
101 |
77.95% |
22.05% |
|
31-40 |
321 |
231 |
90 |
71.96% |
28.04% |
|
>40 |
168 |
125 |
43 |
74.40% |
25.60% |
|
Marital Status | |||||
|
Married |
406 |
328 |
78 |
80.79% |
19.21% |
|
Unmarried |
478 |
381 |
97 |
79.71% |
20.29% |
|
Divorced or Widow |
127 |
48 |
79 |
37.80% |
62.20% |
|
Not known |
46 |
27 |
19 |
58.70% |
41.30% |
|
Education Status | |||||
|
Illiterate |
526 |
412 |
114 |
78.33% |
21.67% |
|
Primary |
288 |
206 |
82 |
71.53% |
28.47% |
|
Junior |
173 |
112 |
61 |
64.74% |
35.26% |
|
Senior |
47 |
38 |
9 |
80.85% |
19.15% |
|
College |
14 |
9 |
5 |
64.29% |
35.71% |
|
Unknown |
9 |
7 |
2 |
77.78% |
22.22% |
|
Transmission route | |||||
|
Sexual route |
218 |
180 |
38 |
82.57% |
17.43% |
|
Injecting drug |
524 |
443 |
81 |
84.54% |
15.46% |
|
Blood transfusion |
112 |
73 |
39 |
65.18% |
34.82% |
|
Unknown |
203 |
88 |
115 |
43.35% |
56.65% |
Comparative representation of clinical analysis andmedical history of HIV positive TB patients and HIV patients with otherco-infections
|
Variable |
HIV+TB |
HIV+ other Co-infections |
|
Fever |
83% |
64% |
|
Cough |
77% |
67% |
|
Short Of Breathes |
67% |
48% |
|
Weight Loss |
66% |
60% |
|
Diaphoresis |
47% |
39% |
|
Cachexia |
36% |
15% |
|
Symptoms >2 Week |
40% |
67% |
|
Diabetes mellitu |
9% |
15% |
|
Sputum |
73% |
70% |
|
Alcohol Use |
33% |
30% |
|
Immuno-compromised |
17% |
30% |
|
Other Drug User |
78% |
47% |
|
History Of Tb |
31% |
11% |
|
Time Duration (Months) |
8-11 |
14-18 |
HIV and Co-infections
In the present study, the investigation of HIV patients for co-infections revealed that out of 1057 HIV patients, 82 were not suffering from any co-infection, while the majority of patients were suffering from a co-infection of HIV + TB (347) and HIV + HBV or HCV (201). A significant number of HIV patients with a co-infection with Malaria and typhoid were also detected (198 and 155, respectively). Few immune compromised HIV patients had typhoid and HPV infections as well (Figure 1).
Level of CD4 cells
Individuals infected with HIV had 221.3±19.3 cell/mm CD4 cells, however, in HIV + TB co-infected patients, the amount of CD4 cells dropped to the lethal stage (107.4±29.2 cell/mm3). Co-infection of HBV and HIV or HCV also significantly reduced the CD4 level in infected patients (144.7±33.6 cell/mm). Patients suffering from AIDS and co-infection of typhoid, HPV, and Malaria also negatively affected CD4 levels in patients (Figure 2).
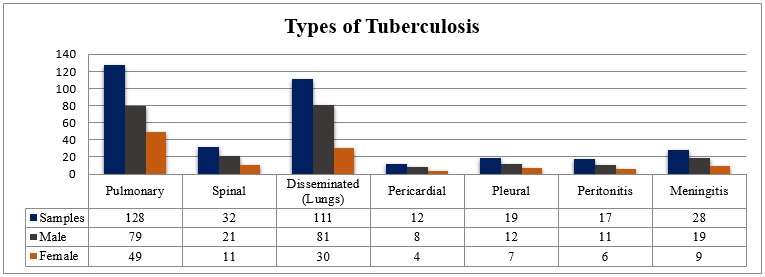
Types of Tuberculosis in HIV patients
In current research work, out of 1057 HIV patients, 347 suffered from a co-infection of HIV + TB. The radiological analysis revealed that lungs were more damaged as most HIV patients were suffering from pulmonary TB and disseminated (lungs) TB (128 and 111, respectively). Spinal and meningitis TB was also detected among patients (32 and 28, respectively) (Figure 3).
Area of HIV patients
According to figure 4, most HIV patients were Afghan refugees or those Afghanis who came to Pakistan for better treatment in hospitals of KPK (386, 37%). Similarly, in the area of Pakistan near to Pak-afghan border, FATA (Federally Administered Tribal Areas) was also affected with HIV (278, 26%). 13% of patients belonged to Kohat, and 11% from Attock, KPK, Pakistan. In addition, due to homosexual interaction among prisoners, 7% of prisoners were suffering from AIDS.
DISCUSSION
Pakistan is one of four Asian nations where HIV prevalence has increased over the last decade. Over the same time frame, the number of new HIV infections increased from 14000 in 2010 to 22000 in 2018, resulting in a 368 % rise in HIV-related fatalities with male domination22, 23. Even though HIV is largely confined to specific populations, Infections have previously emerged in the general population24, 25. The present study has comprised a total of 1057 HIV patients. Males made up 74.14 % of the 1057 HIV patients, with most of them aged 21 to 30. The patients that were infected were mostly unmarried and uneducated. Another group of causes that could be leading to an elevated risk of HIV contamination in terms of sexual activity is social tension and a high prevalence of drug addiction26. Previous accounts of recurring sexual assault, early age suicide attempts, and clinical distress indicate psychological stress 27. While Vertical propagation might potentially be a factor, it is generally thought that the parenteral spread of HIV by the misuse of needles in healthcare settings is to blame for the epidemic25, 28. In the current investigation, the most common viral transmission routes in patients were injecting drugs using contaminated syringes and having sexual connections with infected people (
The rise of HIV has increased the global burden of tuberculosis. As a result, HIV infection greatly raises the risk of contracting active tuberculosis. In the fight against tuberculosis, the T-lymphocyte subset is crucial. Ironically, HIV depletes CD4+ T-lymphocytes, making co-infected people more susceptible to tuberculosis 29. Co-infection with HIV and tuberculosis (TB), also known as the "cursed duet," is becoming a significant public health issue in Sub-Saharan Africa, where 70-80 % of HIV-positive patients also have TB30. The immunological, virological, biochemical, and elastographic responses of patients co-infected with HIV and HBV or HCV and their development and prognosis are not well understood31, 32. Cirrhosis and end-stage liver disease occur as a result of insufficient immune responses to the hepatitis viruses in co-infected individuals 33, 34, 35. HIV co-infection is related to hepatitis flaring after ART treatment and is responsible for a greater risk of death than HCV or HBV infection only36, 37. The analysis of HIV patients for co-infections indicated that 82 had no co-infections, while most patients had a co-infection of HIV + TB (347). A significant proportion of HIV patients were also found to have co-infections with HCV, Malaria, and Typhoid (Figure 1).
The level of CD4 cells decreases when an HIV infection progresses and exposure to any other co-infection11, 38. In different articles, it has been noted that clinical and radiologic manifestations in HIV patients are different reliant on the level of immunity suppression in different patients 12, 39, 40. In such a way, in different reports, it has been pointed out that in CD4 counts of less than 200, atypical manifestations are present and also called killer stage 12, 41, 42. In the current study, individuals infected with solely HIV had 221.3±19.3 cell/mm CD4 cells, whereas HIV + TB co-infected patients had 107.4±29.2 cell/mm CD4 cells (Figure 2).
Unlike other HIV-associated adaptive infections, tuberculosis can strike at any stage of immunosuppressant patients, while its occurrence up to level rises in patients with extra immunesuppression43, 44. Pulmonary tuberculosis is diagnosed using prolonged signs, chest X-ray differences, sputum smear, and culture, but approximate diagnosis can be challenging because clinical and radiological results can be non-specific, particularly in HIV-positive patients. However, in resource-limited nations, most pulmonary tuberculosis diagnoses are made using chest X-rays and clinical features45, 46. Most HIV patients had pulmonary TB and disseminated (lungs) TB (128 and 111, respectively). Therefore the radiological investigation indicated that the lungs were more affected. HIV Patients with spinal and meningitis TB was also detected (Figure 3).
The chest radiography detection of pulmonary tuberculosis in advanced HIV infection is apparently unlike associated with persons with fewer severe immunosuppression47. The lower lobe of the lung, middle lobe of the lung, interstitial fluid, lungs exudates, and pleural effusion and intrudes is mutual, and cavitations are very few 48, 49. However, other radiographic findings, such as pleural effusion, were less prevalent in our HIV-positive individuals than other studies, suggesting that atypical radiological presentations of PTB are common in HIV-positive participants.
The use of inhaled and injected drugs, multiple sex habits, men who have sex with men (MSM), and interaction with sex workers may increase the risk of contracting HIV among refugees and foreigners 50, 51. According to a Pakistani survey, 54% of migrant men engage in unprotected sex, with only a handful using condoms50, 52. A connection between HIV infection and population displacement (refugees and internally displaced people) from conflict/war-affected areas has been identified50. The present study shows that most HIV patients were Afghan refugees or Afghans who had come to Pakistan for better treatment at KPK institutions (386, 37%) (Figure 4). Similarly, HIV was found in FATA (Federally Administered Tribal Areas) in Pakistan near the Afghan border. AIDS has also infected 7% of prisoners due to homosexual activity. MSM is believed to account for 5–10% of all new HIV infections worldwide53. Evidence suggests that this population is more susceptible to HIV infection 53, 54. It is important to remember that Pakistani culture does not support the presence of MSM, which may explain why data on MSM and STDs in the country are scarce.
CONCLUSIONS
It is concluded from the current study that young single and illiterate males were more affected by HIV and TB, due to sexual contacts and injecting intravenous drugs by contaminated syringes. As compared to other co-infections, the patients with co-infection of TB and HIV were more affected demographically and clinically, such as high fever, shortness of breathing, Diaphoresis, Cachexia, and extreme cough. Radiography was abnormal and pulmonary TB was common in HIV-positive TB patients. Co-infection of HIV and TB significantly reduced CD4 cells level in patients (less than 82-124, killer stage) The majority of HIV patients were Afghan refugees or those Afghanis who came to Pakistan for better treatment in hospitals due to unprotected sex or homosexuality. HIV adversely affects the human body's immune system and opens pathways for other microbial infections; therefore, it is a risk factor for TB and the cause of HBV, HCV, typhoid, diarrhea, HPV, and many more.
List of abbreviations
HIV Human immunodeficiency virus
TB Tuberculosis
CD4 Cluster of Differentiation 4
AFB Acid-fast bacilli
AIDS Acquired Immune Deficiency Syndrome
WHO World Health Organization
HCV Hepatitis C Virus
HBV Hepatitis B Virus
HPV Human Papilloma Virus
MSM Men who have Sex with Men
STDs Sexually Transmitted Disease
Ethical Approval
Kohat University of Science and Technology in Pakistan, Shaheed Benazir Bhutto Women University in Peshawar, Pakistan, Khyber Medical University in Peshawar, Pakistan, and the national AIDS and TB control program in KPK gave ethical approval to the study.
Acknowledgment
The authors are thankful to the patients, staff members, and health workers at Khyber Teaching Hospital, Hayatabad Medical Complex, Kohat Medical College, and Lady Reading Hospital Peshawar, andthe national AIDS and TB control program in KPK, Pakistan for their cooperation throughout the study. The authors are also thankful to the Department of Zoology, Kohat University of Science and Technology, Pakistan,Department of Microbiology, Shaheed Benazir Bhutto Women University, Peshawar, Pakistan,Department of Microbiology, Khyber Medical University, Peshawar, Pakistan for providing research facilities, and the team of Big Bio for their support.
Conflict of interest
The authors declare that they have no competing or conflict of interest.
Authors Contribution
All the authors contributed equally in the conceptualization of the study, data collection and analysis, manuscript writing, and final approval.
Funding
The current study was not supported by any funding agency.

