Omicron: Flighty factor challenging global vaccine campaigns or the ending signal of the COVID-19 pandemic
- VNUK Institute for Research and Executive Education, The University of Danang, Vietnam
- School of Medicine, Vietnam National University Ho Chi Minh City, Vietnam
Abstract
Coronavirus disease 2019 (COVID-19) has been a great global public health issue for two years. In November 2021, a new variant, B.1.1.529, of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in South Africa and caused a rapid rise in COVID-19 cases. On 26 November 2021, the World Health Organization (WHO) named this variant Omicron and classified it as a variant of concern (VoC). The spike protein of this variant contains a high number of mutations, raising concerns about viral transmissibility, pathogenicity, immune evasion, and neutralization by antibodies. When the early Omicron surge occurred, preliminary data showed that the transmission of this variant was extremely fast, but the number of patients with severe symptoms was low. This review will describe the characteristics of the Omicron variant and compare the mutations of the spike in the five VoCs. We also look over research and opinions on the Omicron variant and evaluate epidemiological data from the Omicron wave and the Delta wave. In the review discussion, we will discuss Omicron whether it is a challenge for global vaccine campaigns, whether it is a sign of a waning pandemic, and how we acknowledge the new variant and future of the COVID-19 pandemic.
Introduction
Two years after the outbreak of the COVID-19 pandemic, which resulted in nearly 500 million cases and 6.1 million deaths, the world is still on high SARS-CoV-2 alert1. In December 2020, the Delta variant (B.1.617.2) was identified and spread quickly worldwide. The dominance of the Delta strain at that time was associated with a longer duration of infectiousness, higher viral load, and high rates of reinfection because of its vaccine-induced immunity2, 3. Soon after, the Delta variant became the main variant causing the outbreaks in the summer of 20214, 5. On 26 November 2021, the World Health Organization (WHO) declared the B.1.1.529 strain of COVID-19, detected in South Africa, to be a variant of concern (VoC) and named it Omicron6. Scientists are scouring patchy evidence from around the world to better understand Omicron. A few months after the alert from WHO, Omicron has been becoming the dominant variant, and the number of new cases is constantly increasing. The rapid transmissibility of Omicron raises many questions. The main concerns about Omicron are whether it is more severe than other VoCs, whether it can circumvent vaccine protection and whether it is a sign of a waning pandemic. This review examines research as well as opinions on the Omicron variant and interpret its implications for the pandemic in the future.
An overview of the Omicron variant
The new variant of SARS-CoV-2, Omicron (B.1.1.529), was first reported from South Africa on 24 November 20216. Mahmoud Kandeel conducted Omicron phylogeny by using various evolutionary alternative models to compare and analyze genome sequences of SARS-CoV-2 variants. For the nucleotide substitution models, the results showed that the Omicron variant established a new monophyletic clade far different from other SARS-CoV-2 variants7. However, the basic nucleotide substitution model indicated that Omicron and Alpha variants might have a close origin, with the fewest nucleotide alterations of all the analysis variants7. This result suggested that the Omicron variant could exist for a long time in the community until it was identified.
Compared to the original variant, more than 60 mutations have been identified in the Omicron variant, including 50 nonsynonymous mutations, eight synonymous mutations, and two noncoding mutations8, 9. Among the deletion mutations reported, three amino acids (3674-3676) found in the Omicron sequence have been suspected to cause immune evasion10. Three deletion at positions 27-29 were also identified in the accessory protein ORF9b. Additionally, ORF9b is believed to suppress the innate immune response to viral infection and induce IFN production11, 12. Another 30 point mutations were found in the spike, of which half were mutations in the receptor-binding domain (RBD). A cluster of mutations, including H655Y, N679K, and P681H, was identified in the furin cleavage site of the spike protein13. As reported in previous research, these mutations may increase transmissibility and allow the virus to bind to the angiotensin-converting enzyme 2 (ACE2) receptor on host cells9, 14, 15. The D614G change in spike has been observed in all five VoCs, a significant concern because D614G is an amino acid that contributes to the higher upper respiratory tract viral loads in younger patients16, 17, 18. The N501Y mutation on the Omicron variant was also found in Alpha, Beta, and Gamma variants, which was reported to increase the binding of spike and ACE2, therefore inducing higher transmissibility19. It is suggested that all the mutations of Omicron could enhance the virus's infectivity and consequently cause a rapid infection rate.
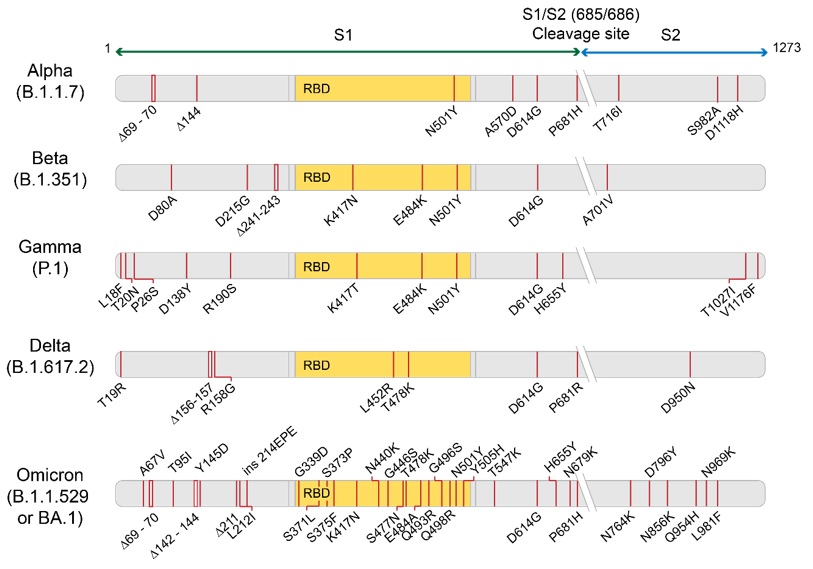
Diagram showing mutations in the spike protein (subunits 1 - S1 and subunits 2 - S2) of five VoCs, including Alpha, Beta, Gamma, Delta, and Omicron
Since the first case was reported in South Africa, some analyses and studies have been conducted to examine and evaluate whether the genetic change of Omicron implicated transmissibility, severe illness, or vaccine efficacy. Several studies have shown that the binding free energy (BFE) between the spike protein and ACE2 positively correlates with viral infectivity20, 21, 22, 23, 24. In the research of Chen , an artificial intelligence model was used with tens of thousands of experimental data points to analyze the BFE changes of the ACE2-spike protein complex in 15 Omicron RBD mutations and examine the infectivity of Omicron25. The results suggested that Omicron is ten times as infectious as the original strain and approximately two times more contagious than the Delta variant. Based on the 3D structure of the antibody-RBD complex, the Omicron variant was more than twice as likely to escape the immunity generated by the vaccine compared to the Delta variant. The research of Ford showed that the affinity of Omicron’s RBD for neutralizing antibodies was reduced compared to the wild-type RBD structures26. The SARS-CoV-2 Omicron variant can escape vaccine immunity based on the spike protein. Although more and experiments are needed to validate these predictions, this study hints at focusing on the vaccine and drug design in the future as well as mutational investigation in new variants. These preliminary studies suggested that the Omicron variant had a high infectious rate because its spike protein mutations increased the interaction with ACE2 and evaded vaccine immunity.
Unpredictable variables or positive signs?
Since the first case of SARS-CoV-2 was reported, we have gone over milestones in the COVID-19 pandemic. The world has witnessed great losses, with more than 5.6 million deaths from COVID-19, and many other illnesses have suffered due to an overloaded health system1. Remarkably, there are many encouraging results in efforts to repel COVID-19, namely, research and development of vaccines and antiviral drug vaccination campaigns in countries and booster dose programs. One year after the vaccination program started in December 2020, approximately 60% of the worldwide population was fully vaccinated1, surpassing the WHO target of 40% coverage by the end of December 20216. This achievement was a collaborative effort of many countries and vaccine developers, funders, and donors27. However, there were still inequities in vaccination coverage between developed and developing countries despite the efforts of the Vaccines Global Access (COVAX) program to roll out fair and equitable vaccines for all countries. While the average vaccine coverage was 60% of the European population, only 6% of Africa were fully vaccinated28.
In addition to preventing the spread of the pandemic with a large-scale vaccination campaign, antiviral drugs were considered an effective tool and were simultaneously developed for COVID-19 treatment. Scientists have found that ACE2, transmembrane protease serine 2 (TMPRSS2), spike protein, RNA-dependent RNA polymerase (RdRp), angiotensin AT2 receptor, chymotrypsin-like protease (3CLpro), and papain-like protease (PLpro) could be the main targets for antiviral drug development29. The emergence of antiviral drugs would reduce hospitalizations and deaths and minimize the burden on the healthcare system. In previous pandemics (SARS2003 and MERS2012), broad-spectrum antiviral drugs, including remdesivir and lopinavir/ritonavir, were effective antiviral agents. In the COVID-19 pandemic, interferon-β ha been used for COVID-19 treatments30. Recently, two oral antivirals from Pfizer and Merck & Co. have been proven to lower the risk of hospitalization or death. On 4 November, Molnupiravir, which was developed by Merck & Co, was first approved in the United Kingdom for COVID-19 infection treatment31, 32. The company announced that Molnupiravir (Lagevrio) could halve the risk of hospitalization in mild and moderate COVID-19 patients33. Lagevrio interferes with viral replication, preventing the virus from multiplying and keeping the viral load low. Consequently, Lagevrio reduces the severity of the disease31. Another oral antiviral candidate, Paxlovid, was authorized for emergency use by the FDA on 22 December32, 34. Based on clinical data from the EPIC-HR study, the proportion required to reduce the risk of hospitalization or death of paxlovid was 89%35. Paxlovid consists of nirmatrelvir, a novel main protease (M) inhibitor that blocks SARS-CoV-2 M and stop the virus from replicating, and ritonavir, which slows down nirmatrelvir’s breakdown34. Therefore, nirmatrelvir could exist at higher concentrations and for a longer time in the human body34. Oral antivirals could provide a cheaper and easier-to-administer option for nonhospitalized patients32. With the approval of antiviral drugs, there would be additional tools to fight against the global pandemic.
Since Omicron was first detected in South Africa, it has spread rapidly, increasing the number of infected patients in the country. Immediately on 26 November, the WHO announced Omicron as a VoC and warned countries to take public health and social measures to reduce their risk of COVID-19 and enhance surveillance for a better understanding of the virus circulation6. According to South Africa’s National Institute for Communicable Diseases (NICD), on 1 December, South Africa had over 8,500 cases36. When Omicron was detected in South Africa in late November, the NICD determined that the effective reproduction number (R) was above 2 in Gauteng37. This value was below one in September, when Delta was the dominant variant, and the number of infectious cases was falling. The data from GISAID showed that in the Beta variant, the infection rate increased to nearly 50% within 100 days, while the rate of Delta was 80% in the same period5. The infectious rate reached 90% for the Omicron variant within 25 days. These data suggested that Omicron is likely more contagious than the Delta and Beta variants. According to a study by Hiroshi Nishiura, based on epidemiological data in South Africa as of 26 November, the Omicron variant was 4.2 times more infectious than the Delta variant38. With the appearance of the Omicron variant, many countries placed a travel ban on visitors from Africa to limit the global spread of Omicron39. However, until 13January, 142 countries reported cases of Omicron40. Public health authorities in Denmark and Norway released an alert for the coming wave of the Omicron variant, and it has dominated in both countries41, 42. Despite very high vaccination rates, Denmark reported more than 6,000 cases per day, roughly twice the number seen during the highest previous peak. This new variant also caused approximately 73% of cases in the US and rapidly ate into Delta’s dominance43. In the UK, Omicron cases doubled every two days31. However, because not all tests were sequenced, the actual number of Omicron cases might be higher in the population. To handle the situation, the US and Europe proposed urgent lockdown policies and mask mandates to resist the Omicron variant rate of transmission, especially during the Christmas holidays44. By the end of 2021, countries around the world were still reporting a rapid rise in SARS-CoV-2 cases. At another tragic moment of the pandemic, places that saw a surge of the Omicron, reporting of new infections have started to level off or decline1. The slowing of the spread was great news, raising the prospect that a peak in the Omicron wave may be approaching. Nevertheless, most countries continued to see explosive growth in virus cases.
Omicron spread at unprecedented speed, a new threat for vaccination campaigns and vaccine developers. Since this variant had over 30 mutations in the spike protein alone compared to the original virus, it seemed to significantly evade immunity generated by vaccines when antibody levels dropped in the blood. A few studies on Omicron’s ability to escape immunity have been conducted, although these works have not yet been peer reviewed. The research by Wilhelm reported that the neutralizing efficacy of vaccinated serum was reduced with Omicron compared with Delta45. In particular, the serum of people injected with two doses of BNT162b2 and three doses (sampling 0.5 and 6 months after the booster) showed reduced neutralization of 11.4, 37.0, and 24.5 times Delta, respectively. The Omicron neutralization capacity of serum from infected and vaccinated individuals was reduced by 32.8 times compared with that of Delta. Similarly, the study of Rössler reported that serum from vaccinated individuals was the least neutralized B.1.1.529 variant compared to other variants 46. In a study by Andrews , the effectiveness of two doses of the Pfizer or AstraZeneca vaccines in Omicron fell to 40% within 15 weeks after the second dose47. Other preliminary studies from South Africa, Israel, and France also showed a marked decrease in Omicron-neutralizing antibodies in individuals who received two doses of Pfizer or Moderna48, 49, 50, 51. This situation was a challenge for vaccination campaigns around the world. Additionally, there was a strong argument for getting boosters vaccinated. According to Pfizer and BioNTech, three doses of Pfizer increased the neutralizing antibodies 25 times compared with two doses52. As the Omicron variant spreads, the most feasible defense against viral variants was a full dose of a vaccine followed by a booster shot several months later. On the other hand, there are other bold opinions that instead of pursuing booster doses, it is better to research more potent vaccines to protect humans against any new mutations of SARS-CoV-2. A few vaccine developers have confirmed that finding specific variant-tailored vaccines is a new direction in the future52, 53.
The emergence of the Omicron variant raised concerns about a new pandemic wave: Will the Omicron variant be a sign of the end of the pandemic, and will the virus circulate among humans? Preclinical results showed that since the first recorded cases in Africa, although the number of infections increased daily and rapidly54, most of the reported cases had mild symptoms or were asymptomatic. With limited data from South Africa, Omicron variants may cause less severe illness54. Data from hospitals in South Africa showed that between 14 November and 4 December, severe cases reached 6.3%, much lower than in July, when the country faced the Delta variant54. According to the South African Department of Health report, the number of new cases decreased by 29.7% at the end of 2021 compared to the previous week, from 127,753 to 89,78136. Deaths rose by 64% in the first week of 2022 across the continent, mainly among people at high risk. In South Africa, COVID-19 patients occupy only approximately 9% of ICU beds40. In a preprint paper available on Lancet comparing COVID-19 cases in the Gauteng province of South Africa, approximately 4.9% of patients needed to be hospitalized during the fourth wave, compared with 18.9% and 13.7% in the second and third waves, respectively55. The paper also showed that 28.8% of admissions in the fourth wave developed severe disease, lower than 60.1% of the second wave and 66.9% of the third wave55. At the end of December 2021, based on the positive data and indicators, the South African government officially announced that the peak of the fourth wave may have passed at a national level56. In the UK, from 1 December 2021 to 2 December 2021, total new deaths decreased from 1.791 to 1.697 per million, which was a 5% decrease57. Based on limited evidence, Omicron appeared to have a growth advantage over Delta58. It spread faster where Delta circulation was low, such as in South Africa, but its transmission was quicker in the UK, with a higher incidence of Delta59.
A review of official South African COVID countrywide figures from 1 December to 21 December 2021 showed that total deaths increased from 0.466 to 0.583 per million, and new confirmed COVID-19 cases per million population climbed rapidly by 380%57. With many mutations, high transmissibility, and the possibility of evading immunity, the Omicron variant raised concerns about the new pandemic wave. Preliminary findings from South Africa suggested that Omicron variants may be less virulent than Delta variant at some levels59. The trade-off between transmission ability and virulence that occurred in this variant could induce a revolution in the virus’s ability to circulate among humans. Sarah Cobey, an evolutionary biologist at the University of Chicago, said that if the variant spread widely, thanks to the ability of immunity evasion, it would fit into theoretical predictions about the evolution of SARS-CoV-258. According to Cobey, as SARS-CoV-2’s infectivity started to be slow, the virus would overcome immune responses to maintain its fitness. For instance, if a set of mutations halve a vaccine’s blocking transmission ability, this will considerably raise the number of hosts in a population58 and may raise the probability that the virus exists in the human population. Similarly, Adam Kucharski, a mathematical epidemiologist at the London School of Hygiene and Tropical Medicine, said that the most uncomplicated strategy for the virus to emerge into new epidemics was gradually escaping immunity, which was comparable to seasonal viruses58. From those points of view, the evolutionary path of the virus seems to be less virulent.
The Omicron variant spread to many regions, including the US and European countries; however, according to the scientist of NICD, it seemed that the number of new infections had peaked, and South Africa witnessed a decline in new COVID-19 cases (by 20.8% in a report on 22 December 2021)60. According to NICD data, some provinces of South Africa recorded a decrease in cases, and Ridhwaan Suliman, the African Council for Scientific and Industrial Research’s senior researcher, stated that hospitalizations and deaths from this wave have proven to be "significantly lower relative to that experienced in previous waves”60. Although more studies are needed to determine whether Omicron variants are less virulent, there is still hope that the emergence of Omicron will be a "turning point" at the end of the pandemic. WHO officials state that COVID-19 has an end in sight and plan to terminate it in 2022 with all of the tools accumulated over the years, finally making the virus an endemic, which is constantly circulating but not a significant concern61, 62.
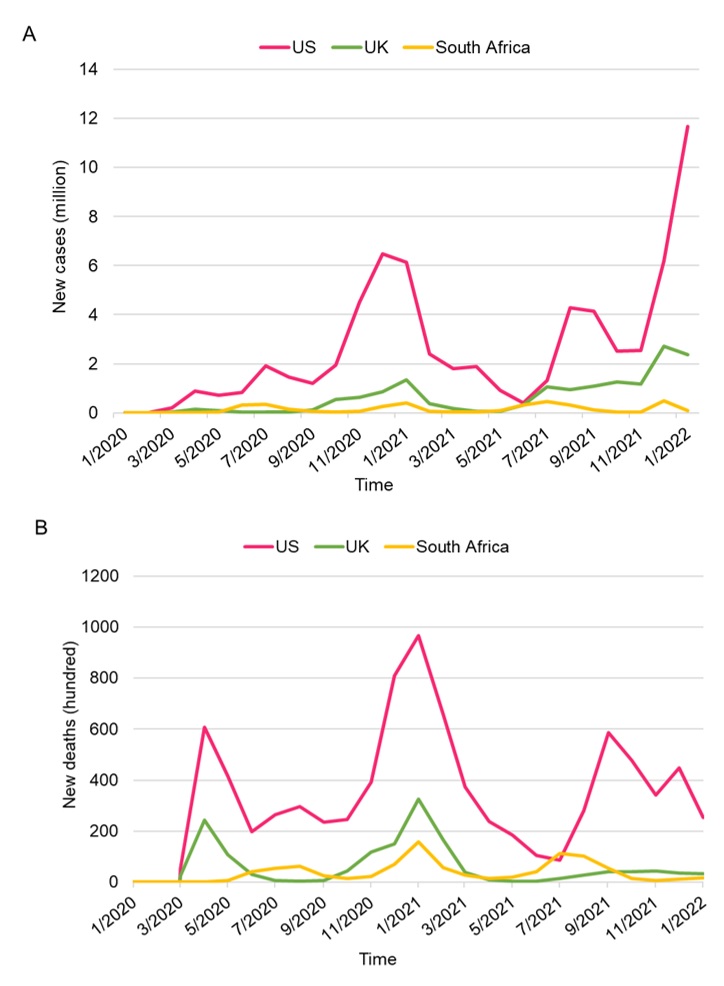
The rolling 7-day average of daily new cases (A) and new deaths (B) from January 2020 to January 2022 in the United States (US), the United Kingdom (UK), and South Africa. The period from June 2021 to October 2021 is the Delta wave. The period from December 2021 to January 2022 is the Omicron wave. To date, Omicron waves are much more contagious, resulting in more cases reported than Delta waves. The 7-day average of daily new cases in the US is more than triple its previous peak, but the number of new deaths is approximately half of its previous peak. Similarly, in the UK and South Africa, the mortality rate during the Omicron wave is lower than that during the Delta surge. The low severity of COVID-19 could have much to do with the innate features of Omicron and the protection generated by the vaccines. The early of Omicron could help countries to give out a roadmap suitable for the new variant epidemic situation. All these factors may also account for fewer deaths in the population.
Discussion
As soon as South Africans identified the new VoC, they warned about the potentially spreading variant. Following the WHO’s revelation of the Omicron variant, many countries have enforced travel bans or travel restrictions to and from countries in southern Africa and neighboring countries39. Many scientists believed that imposing travel bans on a few countries reporting the new VoC Omicron would not prohibit the virus from being imported and limit the spread of major Omicron variant clusters. However, the announcement of Omicron as a VoC and countries’ immediately giving out the travel ban is an effort of the WHO and the government to avoid repeating the mistake with Delta. Look back to the time when Delta was first identified in late 2020. Although the number of new cases in India has increased significantly (recorded over 400,000 cases in 7 days), the Delta variant was not recognized as a VoC until four months later. It took Delta ten months to transmit to 110 countries63, while within just one month from announcing Omicron as a VoC to 22 December 2021, Omicron reached this number64. During the last week of December 2021 and early 2022, many countries reported a record increase in cases due to the Omicron variant. As of 31 December 2021, the UK had 246,000 new cases due to the Omicron variant, much higher than in July of the previous year1. The Omicron variant quickly spread in the US and fueled an increase in infections, averaging more than 267,000 new cases per day1. Although the transmission of the Omicron variant is notably fast, the number of hospitalizations and deaths are much lower in the Delta surge. A preliminary study in the US reported that the Omicron results were notably lower than half those in the Delta65. During the early Omicron surge, the ICU dropped to 5%, and the risk of being hospitalized dropped to 2%, which is an approximately 70% and 50% decrease compared to the data in the Delta wave, respectively. The UK Health Security Agency estimated that individuals infected with Omicron were half as likely to visit or be admitted to the hospital than those infected with the Delta variant66. In addition, individuals who had received two doses of vaccine had a 65% lower risk of hospital admission than those who had not received any vaccination, and those who had received booster doses of vaccine had an 81% lower risk. Therefore, the border closures were too late, and the variant has been detected on every continent, but this gives more time for countries to accelerate vaccination, booster doses, prepare the health system infrastructure and carry out the schedule before the wave of Omicron hits. According to Aris Katzourakis, a viral evolution researcher at the University of Oxford in the UK, the Omicron variant still had an advantage when infecting a highly vaccinated population that gave up on other control measures67. Rather than prohibiting people from traveling, it was preferable to strike a balance between lifting restrictions and resuming travel while still taking the required actions to address the intricate progression of the pandemic. To limit the risk of the Omicron from being imported or exported, government agencies of departure, transit, and arrival may apply a multilayered approach or quarantine.
While 60% of the population in Europe has received COVID-19 vaccinations, just 5-10% of the population in Africa has received the first dose (24% in South Africa)39. Only approximately one-fifth of Africans were entirely immune to COVID-19. These factors contributed to the emergence of VoCs, and the more people who were vulnerable to SARS-CoV-2, the greater the chance for the virus to circulate and transmit into the human body. As a result, the virus evolves, eventually leading to vaccine-resistant variants. The lack of vaccination coverage further prolongs the outbreak, placing the entire world at continuous risk of COVID-19. On the other hand, the appearance of VoC Omicron nearly two years after the COVID-19 virus’s first discovery serves as a clear reminder that the COVID-19 pandemic was far from over. The emergence of Omicron variants once again caused a debate on whether a booster is needed. A booster dose is an additional dose used to provide better protection to fully vaccinated people. Data from Israel68, 69, 70 and the UK47 indicated that a booster dose from mRNA vaccines significantly reduced the risk of catching SARS-CoV-2 and getting sick. The level of the antibodies fell over time after vaccination, reducing their ability to control infection waves. If Omicron turned out to be highly communicable, the booster might be helpful due to its proclivity for eliciting a broad array of antibodies. Extra vaccination doses might restrict viral spread by increasing the quantity of “neutralizing antibodies” that directly block the virus from entering cells if community transmission rates remain high71. A variation-specific booster will be available shortly. However, in the meantime, current vaccines such as Pfizer-BioNTech52 or Moderna72 booster have been more successful than the last two shots at neutralizing antibodies against the Omicron variant. Large companies are also developing new, more effective vaccines with Omicron in conjunction with boosters and have shown many positive results. Pfizer indicated that a vaccine targeting the Omicron variant should be ready by March 2022. These new vaccine can be updated to address any future variant of potential concern if needed. If the present vaccination's booster dosage fails to defend against the Omicron variation or any future variants, the ability to formulate and manufacture a variant-specific vaccine in less than 100 days is astounding73. New vaccines such as protein-based vaccines might become more widely available due to their lower price and less stringent storage requirements than mRNA vaccines currently do. In December, the WHO approved a protein vaccine made by Novavax for emergency use74. Other approaches are also being considered, such as the new CanSinoBIO’s inhaled COVID-19 vaccine75 and another developed by Bharat Biotech76. These vaccine are a needle-free, noninvasive treatment that seeks to deliver rapid, consistent, and widespread protection with simple administration77.
There were clear indicators that Omicron is more transmissible than the previous Delta variant, and early evidence suggests that it is also less severe, which are ideal circumstances for any virus to transition from epidemic to endemic stage71. According to Pfizer's chief scientific officer, Mikael Dolsten, when and how this happens will be determined by the disease's progression, the effectiveness with which society deploys vaccines and treatments, and, once again, equitable distribution to areas with low vaccination rates74. High transmissibility is a major concern, but it also indicates that the virus has been so well adapted for human-to-human transmission that it will never disappear. Rather than scaring ourselves, people would have to learn how to live with it. Regular vaccinations and antiviral drug treatments could be combined with infection-born immunity to make COVID outbreaks far less severe but instead a cycle of more cases and fewer cases, similar to what happens every year with influenza78. Since Omicron was resistant to a few antiviral drugs, variants identifying SARS-CoV-2 may be needed to select variant-specific agents before prescribing medication. In addition, each individual can prevent the transmission of the COVID-19 virus by maintaining a physical separation of at least two meters between themselves and others, wearing a well-fitting mask, keeping hands clean, coughing, or sneezing onto a tissue or perhaps a bent elbow79.
As time passes, the concept of Omicron as nature's vaccination gains traction. Professor Ian Jones, a virologist at the University of Reading, believes that the newly discovered Omicron can increase immunity without causing major sickness80. Like the flu or a regular cold, Omicron poses a minor threat to healthy and fit people. Some specialists, however, have rejected the notion of Omicron being a natural vaccine. According to Shahid Jameel, a well-known virologist, deliberately exposing individuals to a virus about which there is insufficient information is not proper science, particularly when other factors affecting human health and vaccine reception, such as malnutrition, air pollution, and diabetes, are taken into account, especially when considering his own country, India, and several others80. Furthermore, a new drug must be required for those who have severe sym toms after being exposed to Omicron. Even though new drugs are discovered regularly and, theoretically, other drugs that target nonmutated sites of the virus might still work81, 82, the high transmission rate of variants would inevitably burden the health system in terms of providing support to everyone.
Comparison of delta and omicron variants in biological and epidemiological characteristics, vaccine efficacy and drug efficacy.
|
Delta/B.1.617.2 |
Omicron/B.1.1529 |
Reference | |
|
Biological and epidemiological characteristics of Delta and Omicron variants | |||
|
Spike protein mutations |
10 |
30 |
|
|
Transmissibility |
Medium |
High (the risk of being infected by Omicron is more than double compared to Delta) |
|
|
Severity |
High |
Low (approximately 60% lower risk of hospital admission and a 70% lower risk of death) |
|
|
Vaccines efficacy against Delta and Omicron variants | |||
|
Pfizer Comirnaty (BNT162b2) |
82% Booster dose: 91.8 - 94.9% |
48.7% Booster dose: 55.0 - 64.4% |
|
|
AstraZeneca (ChAdOx1 nCoV-19) |
67.0% Booster dose: 83.3 - 94.9% |
28.6% Booster dose: 46.7 - 60.9% |
|
|
Moderna (mRNA 1273) |
80.2% Booster dose: 94.7 - 96.4% |
44.0% Booster dose: 64.9 - 66.3% |
|
|
Efficacy of monoclonal antibodies and antiviral drugs against Delta and Omicron variants (in vitro study) | |||
|
Molnupiravir |
Effective |
Effective |
|
|
Nirmatravir |
Effective |
Effective |
|
|
Remdesivir |
Effective |
Effective |
|
|
Etesevimab |
Effective |
Reduced |
|
|
Imdevimab |
Effective |
Reduced |
|
|
Sotrovimab |
Effective |
Effective |
|
|
Casirivimab |
Effective |
Slightly reduced |
|
Conclusion
To date, we are still facing many challenges from COVID-19. The appearance of the Omicron variant, which has more mutations than previous VoCs, might make it complicated to predict. It is still a big question whether it is severe and circumvents vaccine protection or a sign of a waning pandemic. The current epidemiological data on the frequency of hospital admissions and fatalities related to the Omicron variant are not too high, and most infectious patients are asymptomatic. However, studies and data on SARS-CoV-2 and Omicron are still preliminary. Therefore, because of concern about the spread of this variant, implementing vaccine campaigns and regulations such as wearing masks in public, using disinfectant solutions, and limiting crowded gatherings are still necessary.
List of abbreviations
3Clpro: Chymotrypsin-like protease
ACE2: Angiotensin-converting enzyme 2
BFE: Binding free energy
COVAX: COVID-19 Vaccines Global Access
COVID-19: Coronavirus disease of 2019
EPIC-HR: Evaluation of Protease Inhibition for COVID-19 in High-Risk Patients
EU/EEA: European Union/European Economic Area
FDA: Food and Drugs Administration
MERS: Middle East respiratory syndrome
NICD: National Institute for Communicable Diseases
Plpro: Papain-like protease
RBD: Receptor binding domain
RdRp: RNA-dependent RNA polymerase
SARS: Severe acute respiratory syndrome
SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2
TMPRSS2: Transmembrane protease serine 2
UK: United Kingdom
US: United States
VoC: Variant of Concern
WHO: World Health Organization
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
This research was funded by the VNUK Institute for Research and Executive Education, The University of Danang under grant number T2021-VNUK-02.

